by Connie Kent
For a medical crises, we know to dial 9-1-1. But what about medically related crises that aren’t emergencies? In January I approached Father Joel to discuss a perceived need. A couple of residents I knew, both living independently in cottages, were recently unable to get the care they thought should have been available to them from the Manor following medical procedures which left them temporarily disabled. My question to Father Joel: Who should residents turn to for help in dealing with such a crisis? These residents felt they were abandoned when they had been led to believe the Manor’s promised “Continuum of Care” would provide the services they needed. Other crises that might need such a resource are a devastating diagnosis, the need for help for a spouse whose health is failing, or the sudden death of a partner.
How can we help each other, living together as we do, at this point in our lives? One way is to offer our support when we see someone in need. Please see Need Help?
Another way is to develop systems for dealing with our concerns and to make them known. Following the Residents’ Forum Zoom meeting in February, a small Residents Council Ad Hoc committee was formed to address some of the health-related issues I had brought up with Father Joel. Failing to come up with a name for our new committee, we call it The Unnamed Committee. Members include Gary Crites, Gini Armstrong, Dan Wagner, Jan Rowe, Jim Ellis, Joni Johnson, Bob Carter and me. We’ve met several times via Zoom. Here are the topics we have addressed.
1) Issue: One of our residents spent months after he moved in, going from office to office here at the Manor, collecting information about how to help his ailing wife.
Q: What single person or agency here at the Manor should residents turn to in a crisis?
A: In May, at the time of this writing, Debi Watt has told the committee that Resident Services is the office residents should consult when they’re in crisis.
2) Issue: medical transportation. More and more medical procedures are conducted in surgery centers rather than hospitals, and frequently they are scheduled early in the morning, before regularly scheduled Manor Medical Transportation is available at 8 o’clock.
Related is the issue of transportation back home. Following in-hospital out-patient procedures as well as surgery center procedures, patients are routinely discharged while still in need of round-the-clock care. If I am such a patient, I may well be woozie from anesthesia and need help navigating.
Q: How can I get to early morning medical procedures? And will Medical Transportation pick me up and see me safely back to my unit?
A: This issue has been turned over to the Health Services Advisory Committee, which is currently evaluating the extent of the need. Their assessment should be available in 60 days.
3) Issue: If I am discharged to a nursing facility and there is room and sufficient staffing in the Health Center, I will be given a bed there. But then there is the issue of cost. In the past, one had to have been hospitalized for at least three consecutive nights in the hospital for Medicare to cover the expense of skilled nursing care.
Q: With more and more out-patient procedures and short or non-existent hospital stays, will Medicare cover the cost of skilled nursing care?
A: Melissa Preston, Health Services Administrator, says that this past year, due to the COVID 19 pandemic and the need to relieve the burden on hospitals, CMS (Centers for Medicare and Medicaid Services) has authorized hospitals to activate waivers that allow for the 3 midnight stay qualification to be waived. She says we have seen it happen several times with our local hospitals, where individuals have been discharged to the skilled nursing facility under this waiver and have qualified for skilled services without a 3 midnight stay. However, the ability to activate those waivers expires soon, unless it is renewed at the Federal level. Ed. note: please refer to Hill Topic‘s “Home Health, Home Care: Support for Vulnerable Times” in the May 2021 issue and “Continuing Care Levels Explained” in the April 2020 issue.
4) Issue: in-home services. Tremendous confusion has existed around what services the Manor provides, in part because of the similarity between the terms “Home Care” and “Home Health.”
Q: If I am returned to my unit, what services are available to me?
A: Melissa Preston gave a very helpful presentation on the difference between Home Care and Home Health. Her presentation is available on the Health Services page of myRVM. Here is a brief summary.
The Manor provides Home Care, primarily to those in Residential Living on an on-going basis but to Independent residents also, for short-term needs, depending on staff availability. Home Care includes help with activities of daily living, meal preparation, companionship, and running errands. It does not include health care. The cost may or may not be covered by one’s insurance.
Home Health services are not provided by the Manor but rather by any one of several outside agencies. Home Health services are typically prescribed by a doctor and provided by licensed personnel such as RNs and therapists. They include such things as administration of medications, wound treatment, IVs, and so on. The cost may be covered by one’s insurance.
5) Issue: end of life planning. If we die without having left information about our affairs and instructions for what to do next, those we leave behind face not only grief but aggravation as well. Even though our own death is a topic we might prefer to ignore, most of us living here can expect to die here. We would do well to prepare for the inevitable while we are most able. This will save our families, friends and the Manor a whole lot of stress.
Q: What do I need to do to ensure that my family and/or my executor knows how to handle my affairs after I die?
A: The Unnamed Committee is currently compiling a document with information your family and/or executor will need. This information includes details about your medical, financial, insurance, and legal contacts and documents as well as a checklist of people and agencies that will need to be contacted at the time of your death. Of course, the information will need to be reviewed periodically and modified as necessary. But the time to take care of it is now.
A-2: Resident Services Director Cynde Maurer and Debi Watt, Resident Services Coordinator, have invited Beth Knorr, Director of Trust Services for Oregon Pacific Bank and member of the RVM Foundation Board, to address residents on “Implementing Your Estate Plan,” which will air on Channel 900 on June 23, 2021, at 10 am. A document listing appropriate information to include in such planning will be made available in advance of that presentation.
6) And now there’s a new wrinkle: Issue: what happens when you’re discharged from the hospital on a weekend, you live in a cottage, and you need at-home care? This issue has not even been brought to the committee yet. Click on the link to see Bob’s Story.

 Security Agency. Traveling with them in Europe are Kira, their 19 year old first born, and her younger brother, Tony. One evening in Paris, Kira and Tony meet a good looking French graduate student named Jacques. Kira is attracted but unfortunately, the family is leaving for Spain the next day. Jacques offers to follow them to Spain and meet Kira in a famous bar he knows of. Jacques is not what he seems and things go downhill for Kira. No spoilers here, but this story has more twists and turns than a curvy mountain road and somebody ends up dead. It is available in large print at the RVM Library as are two of the John Wells series.
Security Agency. Traveling with them in Europe are Kira, their 19 year old first born, and her younger brother, Tony. One evening in Paris, Kira and Tony meet a good looking French graduate student named Jacques. Kira is attracted but unfortunately, the family is leaving for Spain the next day. Jacques offers to follow them to Spain and meet Kira in a famous bar he knows of. Jacques is not what he seems and things go downhill for Kira. No spoilers here, but this story has more twists and turns than a curvy mountain road and somebody ends up dead. It is available in large print at the RVM Library as are two of the John Wells series.




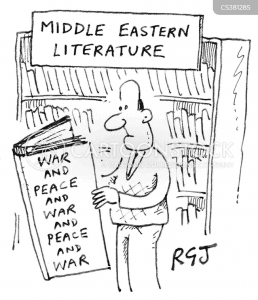 against Arabs or the other way around. But in truth, we Israelis were a proud group of intelligent people who joined together to create a start-up nation and shone with our growth and achievements. I felt safe in the state of Israel, able to walk with my head up and a smile on my face, unlike being in Europe by myself as a Jew pretending not to be one.
against Arabs or the other way around. But in truth, we Israelis were a proud group of intelligent people who joined together to create a start-up nation and shone with our growth and achievements. I felt safe in the state of Israel, able to walk with my head up and a smile on my face, unlike being in Europe by myself as a Jew pretending not to be one.

 I have researched methods of cooking emergency food following a major disaster, when there is no gas or electricity. I was surprised to find that the companies that supply emergency food didn’t seem to have any recommendations on heat source. Many assume you are prepared for living off the grid and have a wood stove or perhaps a white gas stove.
I have researched methods of cooking emergency food following a major disaster, when there is no gas or electricity. I was surprised to find that the companies that supply emergency food didn’t seem to have any recommendations on heat source. Many assume you are prepared for living off the grid and have a wood stove or perhaps a white gas stove.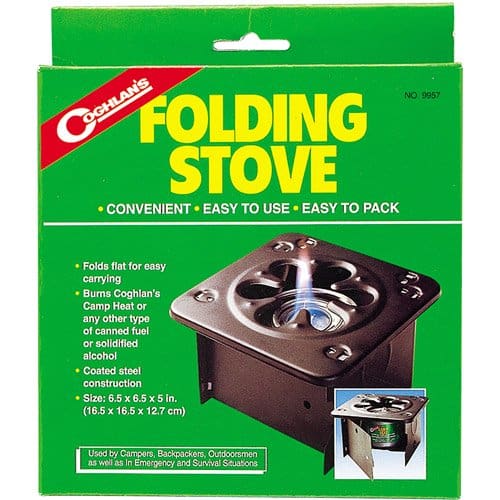


 “Comfort food” is one of the items on many of the lists of what to store in case of an emergency that cuts you off from normal supplies. The idea is that when times are hard, a bit of pleasure can keep you from sinking into terminal depression. A good plan, and for many many people, comfort food is nearly synonymous with chocolate. So there you are, far from home, fleeing a summer wildfire in 100+ degree temperatures. Being a well-prepared person, you have ample warm water to wash it down with, so you reach into your pack for that precious package of chocolate. And as you start to open it, a sticky brown liquid runs out of the wrapper and down your arm. Not good. For your next disaster, take M&Ms — “they melt in your mouth, not in your hand” is a slogan that’s true enough so that during WWII the company’s entire output went to the US military to comfort the troops in sometimes hot locations. And besides, the colors are very cheerful. *Nutritional note– each milk chocolate or peanut M&M contains about 4.7 Calories, so you only have to eat 450 of them to get your daily allotment of 2000 Calories.
“Comfort food” is one of the items on many of the lists of what to store in case of an emergency that cuts you off from normal supplies. The idea is that when times are hard, a bit of pleasure can keep you from sinking into terminal depression. A good plan, and for many many people, comfort food is nearly synonymous with chocolate. So there you are, far from home, fleeing a summer wildfire in 100+ degree temperatures. Being a well-prepared person, you have ample warm water to wash it down with, so you reach into your pack for that precious package of chocolate. And as you start to open it, a sticky brown liquid runs out of the wrapper and down your arm. Not good. For your next disaster, take M&Ms — “they melt in your mouth, not in your hand” is a slogan that’s true enough so that during WWII the company’s entire output went to the US military to comfort the troops in sometimes hot locations. And besides, the colors are very cheerful. *Nutritional note– each milk chocolate or peanut M&M contains about 4.7 Calories, so you only have to eat 450 of them to get your daily allotment of 2000 Calories.

