By Joni Johnson
This article began quite casually. I met Arnold Lum while doing take out at the Manor. Somehow, we started talking about his family and wham, I got really excited about his ancestry. So many people at the Manor come from Hawaii but I had no idea where their roots were before then. Family histories are fascinating because so many of them started elsewhere and so differently from my own.
So here is a bit of his life story. I hope this is the first of many pieces on the lives of our amazing residents. Arnold is from the Canton region of China on his mother’s side and half Hawaiian-half Canton Chinese on his father’s side. His parents met and married on Maui but eventually moved to Oahu. There is even some Persian/Indian background with traders that came to China years before he was born.
But the fascinating part is how they got together at all. Arnold’s great grandfather on his mother’s side, Chun Yook Lum, came to California from China to work on the railroad. He was a man with a dream and lots of fortitude. What started out as a laborer position on the Central Pacific railway turned into a job as a provisioner. This meant that his work required him to find out what was needed to nourish the crew and to get those items bought and delivered. He realized immediately the potential of taking his skills and creating his own company doing the same for the many Chinese who were settling in California but wanted a taste of home.
He eventually settled in San Francisco’s Chinatown and sent for his wife and two boys. While there, like other Chinese, he opened his own cigar factory in what is now South of Market and was very successful.
Unfortunately, his success was short lived in what became of clash of cultures and jealousy. Denis Kearney, an Irishman new to San Francisco, became increasing frustrated by the business acumen and success of the Chinese in the area who he felt were taking away his business options. This frustration turned to rage, and with his gift for gab, he turned this rage into what is called Kearney’s massacre, where Chinese buildings and buildings owned by whites with Chinese workers were burned down in an effort to force the Chinese to leave San Francisco.
https://www.sfgate.com/bayarea/article/1877-san-francisco-anti-chinese-race-riots-11302710.php
Chun Yook Lum lost everything in the fire and decided to abandon his stake in California and move to Oahu. Meeting his newly arrived family, he boarded a steamer to Hawaii where he finally realized his dream of supplying Chinese goods to Chinese immigrants in Hawaii. This time, he provided textiles and implements to the many Chinese working on the plantations.
Arnold’s grandfather on his mother’s side, Chun Kam Chow, was 10 years old when he arrived in Hawaii. He saw the importance of language acquisition and education immediately. He worked during the day as a houseboy to Princess (future and last queen) Liliuokalani and went to school at night to improve his English. In the Princess’s household, Chun Kam Chow’s job was to take care of the then current governor Dominis and his wife. This allowed him to practice his English as he studied away. With his English skills, Arnold’s grandfather acted as a liaison with his father and the English speaking community. Then he was part of group acting as a translator that traveled across the country to Massachusetts to buy a muslin bleaching machine to bring back to Hawaii to whiten textiles so that they could be printed or used as white material.
While in China as a small boy, he was betrothed to a girl of his same age in the Canton region. He had not seen her for years. But the bond still existed, and so at the age of 32, he found himself back in China to fetch his “child bride” who was also 32. Her name was Mark Choy Kan, and Arnold still has strong memories of the grandmother (Popo) that came to Hawaii to live with the family.
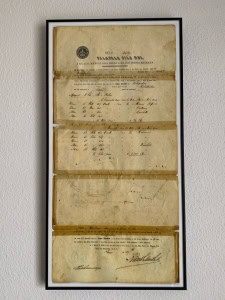
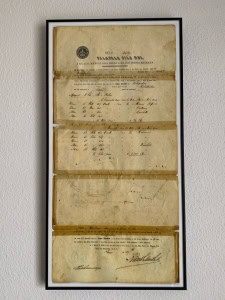
Proof of Taro Patch inheritance
On Arnold’s paternal side, he has both Hawaiian and Chinese blood lines. His grandfather, Ahlo Lum Ling, spent his youth in the Lahaina area of Maui selling silks. In his travels, he would visit the last native village of Hawaii, Kahakuloa, where he met his wife, Kamina’auo. https://www.onlyinyourstate.com/hawaii/time-stands-still-village-hi/ She had inherited a number of taro patches, which made her even more attractive as a mate. So Ahlo spent his time between the beautiful highland town and Lahaina where he had a store. Below is a youtube of Arnold’s cousin singing a song directly from this village.
https://www.youtube.com/watch?v=XiHUjDeirdY

Plaque for Alfred’s work as supervisor of the boarding school.
Arnold’s father, Alfred Lum, was born in 1901 and participated in the then typical six years of schooling before working. On Oahu, he helped build the first road over the mountain – the Pali road. Then he went to work in Maui as a cowboy in the Lahaina Luna, where he eventually became a farm manager and then supervisor of a local boarding school for Hawaiians. There, he was able to teach all sorts of farming tips for maintaining a farm, like how to slaughter an animal properly.
While Arnold’s dad was in Lahaina Luna, Arnold’s mother, Ethel Chun, took a different path. She had loved art all of her life and went to Chiounard Art Institute in southern California and finally on to get her masters degree in art education. But sadly, there were no jobs to be found, and so, magically, she got a job teaching at the same boarding school where Arnold’s dad was in charge. And so love, marriage and children. Hence, Arnold. And finally the family went to Oahu to work for the family business.
While interviewing Arnold, I got to see a number of beautiful paintings that his mother did. But even better, the picture below shows Arnold wearing one of the first aloha shirts that his mother designed. His mother actually designed the very first aloha shirt.

From Arnold, himself:
Uncle Joe (Ellery J. Chun) was my mom’s oldest sib. My grandfather Chun Kam Chow named him Ellery, because Goong Goong (Cantonese familial name for grandpa) read Ellery Queen detective novels in the evening, after the kids were fed and settled.
Uncle Joe was a Yale ‘32 graduate. He disliked his first name and asked the Yalies to call him “Joe”, which was a variant of his middle name. Uncle Joe is consistently referred to as a tailor in the literature about the Aloha shirt, but he couldn’t sew. The backstory is that he was tasked by Goong Goong to develop a business plan for the family store that would capture the growing tourist industry. He decided to start the first mass-printed Aloha shirt production line, which was his first great idea (the second was promoting foreign banking investment in Hawai’i). To prevent imitation, Uncle Joe trademarked the name “Aloha shirt”.
My Punahou schoolmate Dale Hope, author of “The Aloha Shirt”, discovered the trademark when he titled his book. He called me up at work and said “Now what?” I said “go ask Uncle Joe for permission.” The rest, as they say, is history.
Having tasked Uncle Joe with developing a biz plan to market Aloha shirts, Goong Goong asked my mom to design the textile patterns for these puppies. After all, he was paying for the kids’ college educations, having already paid to send five of his brood to Punahou School. So my mom, being the family artist and studying at Chiounard, drew the first textile boards and mailed them back home. These are the boards archived at the Smithsonian Museum of American History (textile dept., second floor of the bldg.).
And so we close our little vignette, fascinated by the family history of one man from Hawaii.










 I was so happy that Jane was there because it took an hour to put the tent up and another hour or so to take the tent down with the both of us trying our best. I don’t know whether the problem was with the tent itself or the damage it had sustained, but the campground had a trash compactor, and my tent was happily disposed of before we left
I was so happy that Jane was there because it took an hour to put the tent up and another hour or so to take the tent down with the both of us trying our best. I don’t know whether the problem was with the tent itself or the damage it had sustained, but the campground had a trash compactor, and my tent was happily disposed of before we left





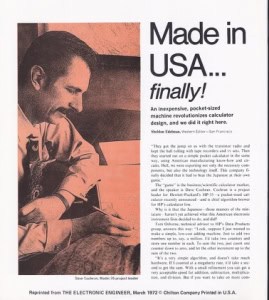
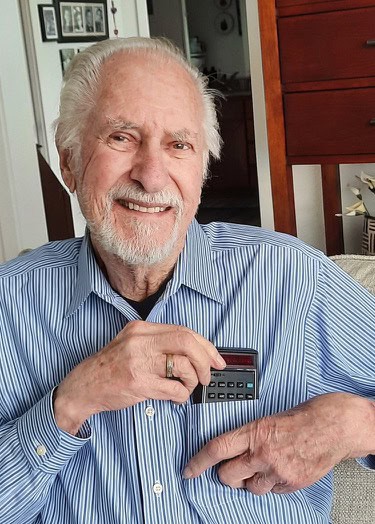 as the man who invented the HP-35 – the pocket calculator that changed the world. One year after its invention in 1972, slide-rules were a thing of the past. While numerous people worked on it, Dave was HP’s Project Chief for the HP-35. Basically, he was responsible for how it looked and how it worked. For his part in the development of architecture and algorithms of the HP-35, he was included in the bicentennial issue of Time Magazine’s “American Ingenuity”. One of the major components of the HP-35 was its use of Reverse Polish notation (RPN). Instead of putting in 8×2=16, you would you hit 8, Enter, 2, X (you still get 16). Dave said that the reason he used this was due to the greater exactness of the equations under study and less chance of ambiguity. People either loved it or hated it, but it was mostly techies who loved it, so ultimately mass marketing demand led HP back to ordinary algebraic formulations.
as the man who invented the HP-35 – the pocket calculator that changed the world. One year after its invention in 1972, slide-rules were a thing of the past. While numerous people worked on it, Dave was HP’s Project Chief for the HP-35. Basically, he was responsible for how it looked and how it worked. For his part in the development of architecture and algorithms of the HP-35, he was included in the bicentennial issue of Time Magazine’s “American Ingenuity”. One of the major components of the HP-35 was its use of Reverse Polish notation (RPN). Instead of putting in 8×2=16, you would you hit 8, Enter, 2, X (you still get 16). Dave said that the reason he used this was due to the greater exactness of the equations under study and less chance of ambiguity. People either loved it or hated it, but it was mostly techies who loved it, so ultimately mass marketing demand led HP back to ordinary algebraic formulations.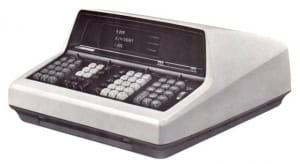 Of course, there would be no HP-35 without Bill Hewlett. He wanted a calculator that would fit inside his desk.
Of course, there would be no HP-35 without Bill Hewlett. He wanted a calculator that would fit inside his desk.